Mental health belongs in EHS programs because stress, fatigue, and psychological factors directly increase injury rates. When workers are mentally impaired, they make the same mistakes as workers who skip safety procedures. But HR-led wellness programs don’t track safety outcomes. EHS professionals need to measure and mitigate mental health as an upstream hazard, not just a benefit.
For years, mental health has been filed under ‘HR’s problem.’ Employee Assistance Programs, wellness initiatives, mental health days. All tucked into benefits packages and handled by Human Resources. Meanwhile, EHS professionals focused on lockout/tagout, PPE, and hazard assessments.
That division is costing you injuries.
A worker who didn’t sleep last night is as dangerous as one who skipped lockout/tagout training. You’d never let the second one near equipment. But the first one? They’re already on your jobsite.
Workers who feel psychologically unsafe are 80% more likely to be injured – National Safety Council (NSC)
How Mental Health Directly Impacts Workplace Safety
The National Institute for Occupational Safety and Health (NIOSH) has been studying the stress-injury connection for over 20 years. When workers are under chronic stress, their bodies stay in a constant state of activation. NIOSH research shows this ‘increases the rate of wear and tear to biological systems.’ When that happens, ‘the risk of injury or disease escalates.’
This is a physiological response, and data from OSHA Worker Fatigue Hazards illustrates what it looks like on the ground:
| Evening Shifts | Night Shifts | 12-Hour Shifts |
|---|---|---|
| 18% higher injury rates | 30% higher injury rates | 37% increased risk |
| vs. day shifts | vs. day shifts | per day worked |
Why Mental Health is an EHS Issue, Not an HR Issue
HR treats mental health as a benefits issue. Wellness programs. EAP access. Mental health days. All good things, but they’re focused on employee satisfaction and retention. EHS needs to treat mental health as a hazard. A direct threat to physical safety. Something you measure, track, and control just like you would any other risk factor on your site.
When an incident happens, and the investigation concludes with ‘human error,’ most teams stop there. But what caused the human error? Was the worker distracted? Exhausted? Under so much stress they couldn’t think straight? That’s the upstream cause and in EHS territory. Both approaches matter. However, if HR’s handling mental health and EHS isn’t tracking the safety impact, you’re missing half the picture.
| HR Approach to Mental Health | EHS Approach to Mental Health |
|---|---|
| Wellness benefit | Safety hazard |
| EAP programs | Incident prevention |
| Employee satisfaction metrics | Injury rate reduction |
| Confidential support services | Risk assessment and control |
| Retention and engagement | Fit-for-duty protocols |
4 Mental Health Risk Factors Driving Your Incident Rates
Mental health conditions don’t show up with warning signs or flashing lights. They show up as near-misses, close calls, and accidents that shouldn’t have happened. Here’s what you’re actually dealing with:
1. Stress & Burnout: Impaired Judgment Under Pressure
Workers under chronic stress aren’t thinking clearly. Stress slows reaction time, reduces focus, and clouds judgment. When stress becomes chronic, it leads to burnout, complete emotional exhaustion, and disengagement from work. NIOSH research shows stressful working conditions drive ‘increased absenteeism, tardiness, and intentions by workers to quit their jobs.’ But before they quit, they’re making mistakes. Burnout reduces morale and contributes to the underlying conditions that lead to incidents.
2. Fatigue & Sleep Problems: Slower Reactions, Higher Risk
The NSC found that workers with sleep problems have a 1.62 times higher injury risk. About 13 percent of work injuries can be traced directly to sleep problems. Workers who regularly get less than five hours of sleep? Their injury rate hits 7.89 per 100 employees. More than three times the average.
3. Substance Use: Direct Impairment and Cognitive Decline
Substance use directly impairs judgment, coordination, and reaction time. Workers dealing with addiction or withdrawal symptoms are at significantly higher risk for incidents. This includes both on-the-job impairment and the cognitive effects of untreated substance use disorders. Substance use affects U.S. industry through lost productivity, workplace accidents and injuries, worker absenteeism, low morale, and increased illness.
4. Psychological Unsafety: Fear of Reporting and Personal Crises
A distracted worker is at higher risk of getting hurt. When someone is dealing with personal challenges, financial pressure, or an untreated mental health issue, their attention is divided. That moment of reduced focus is when hands end up in the wrong place and hazards get missed.
The NSC data should get everyone’s attention: workers who felt their employer discourages reporting were 2.4 times more likely to have experienced a work injury. Workers who feel psychologically unsafe are 80 percent more likely to be injured. Psychological safety plays a crucial role in predicting workplace risk and deserves the same priority as any other safety metric.
Why Leading EHS Programs Are Integrating Mental Health
Leading companies aren’t waiting for federal mandates. They’re bringing mental health into their EHS programs because it works. According to Mental Health America, 99 percent of employers who earned Bell Seal certification in 2025 have integrated mental health into their organizational strategy. This isn’t something HR is tackling on its own anymore; it’s becoming a shared responsibility across departments, with EHS playing a central role.
This shift isn’t about being progressive. Organizations are finally acknowledging a root cause that has been quietly influencing incident trends for years. When you address mental health proactively, you see fewer injuries, stronger morale, and improved overall safety outcomes.
5 Strategic Ways EHS Professionals Can Address Mental Health Risks
You don’t need a massive budget or a total culture overhaul. Start with these strategic actions that leading EHS teams are already implementing:
1. Train Your Frontline to Identify and Respond
Equip frontline supervisors to recognize fatigue, distraction, emotional distress, and substance use signs. NIOSH’s Total Worker Health framework puts supervisor training at the center of the approach. A simple conversation (‘You seem off today. Everything OK?’) can prevent an incident. Build peer support networks too. Workers trust other workers. Peer support programs let trained employees provide confidential support and connect colleagues with resources.
2. Make Mental Health Resources Accessible and Trusted
Employee Assistance Programs only work if workers trust them. Promote 24/7 access. Normalize usage. Make sure leadership talks about it. According to SAMHSA, EAPs that actually integrate with workplace culture get better utilization and better outcomes. Partner with your occupational health team to screen for depression, anxiety, and substance use issues during routine health assessments. Early intervention saves lives and prevents incidents.
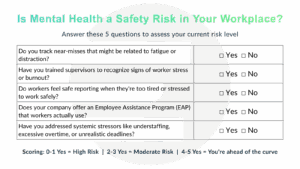
3. Measure Mental Health as a Safety Metric
Add questions about fatigue, stress, and psychological safety to your incident investigations and safety surveys. If you’re not measuring it, you can’t manage it. Track mental health indicators like you track TRIR. Use data to make the business case with leadership. NIOSH research found that stress prevention programs in hospitals led to a 50 percent reduction in medication errors and a 70 percent drop in malpractice claims. Mental health interventions aren’t soft. They’re measurable.
4. Fix Systemic Stressors at the Source
Chronic understaffing, forced overtime, and unrealistic productivity targets all escalate risk on the job and should be treated as safety hazards, not just ‘HR issues’. Work with leadership to identify and fix the root causes driving worker stress. Address the system, not just the symptoms.
5. Build a ‘Fit for Duty’ Culture Without Blame
Workers need to feel safe saying ‘I’m not OK to work today’ without fearing retaliation. Frame it like you would any other safety issue: if you’re not fit for the task, you don’t do the task. Create a culture where reporting mental health concerns is as normal as reporting a physical injury. When workers feel they can speak up without consequences, hazards get caught before they become incidents.
Tools and Resources for EHS Professionals
Here are proven frameworks and tools you can start using today:
- NIOSH Worker Well-Being Questionnaire (WellBQ): Free assessment tool measuring workplace well-being across physical, mental, and organizational factors (cdc.gov/niosh/twh/php/wellbq)
- NIOSH Total Worker Health: Evidence-based framework for integrating health promotion and protection (cdc.gov/niosh/twh)
- SAMHSA Drug-Free Workplace Resources: Complete toolkit for substance use prevention and EAP implementation (samhsa.gov/workplace)
- National Safety Council Workplace Mental Health Resources: Training modules, policy templates, and stigma reduction campaigns (nsc.org/workplace)
- Mental Health First Aid for the Workplace: Evidence-based training to help employees identify and respond to mental health crises (mentalhealthfirstaid.org)
- CDC Workplace Health Promotion: Research-backed strategies and assessment tools (cdc.gov/workplacehealthpromotion)
Mental health plays a direct role in day-to-day safety performance, and it fits naturally within any EHS program. Workers who are struggling psychologically are often the same individuals appearing repeatedly in incident data.
The data from OSHA, NIOSH, and the NSC is clear. Stress, fatigue, substance use, and psychological factors directly drive injury rates. Companies addressing these factors see measurable reductions in incidents, better retention, and improved productivity.
Ready to train your team on workplace safety fundamentals?
Strengthen your approach to Mental Health and Workplace Safety with these courses:
- Drug and Alcohol Awareness for Employees – Identify signs of substance abuse and understand workplace support systems
- Drug and Alcohol Awareness for Supervisors – Best practices for preventing and identifying substance use issues
- DOT Reasonable Suspicion Training for Supervisors – Required training for managers supervising safety-sensitive employees
- Fighting Fatigue in the Workplace – Causes of fatigue, the hazards that it creates and what employees can do to avoid it
Explore eTraining’s complete course catalog→
References: NIOSH, OSHA, NSC, SAMHSA, Mental Health America